Inefficient workflows can cause any business process to falter, and medical processes are no exception. In fact, a streamlined medical office workflow can make or break organizational efficiency.
Whether you’re a private practice, metro hospital, or community clinic, your internal workflow processes form the backbone that drives operational functions within your facility.
What is Medical Office Workflow & Why Does It Matter?
Medical office workflow, or treatment zone workflow, refers to the myriad of tasks, processes, and people that work together to deliver the actual patient treatment.
This precise flow of people and processes directly impacts the patient experience in some pretty obvious ways. Sometimes it takes an outside perspective to see and understand how workflow is affecting the experience.
For example; if your health record system is slow or your team is not fully trained to use all of its features, important details may get lost from visit to visit which causes the patient to get frustrated.

Or, if your internal office communication and notation processes are not clear, the patient may end up repeating themselves frequently within the same visit because their status is not being communicated across your team.
So, How Can You Effectively Streamline Treatment Zone Workflow?
First, Let’s Discuss the Causes of Poor Treatment Zone Workflow
In any given facility, the underlying causes of a poor medical office workflow can be any number of things. However, the most common culprits are:
- Poor Internal Communication
- Inadequate Tools & Technology
- Lack of Training
- Lack of Structure
- Poor Leadership
So, assessing and optimizing these key elements of your office functionality are key to improving workflow, and in turn, improving the patient experience with your facility.
Here are the 6 Steps to Improve Medical Office Workflow Processes
Step 1: Map the Patient Journey
The first, and arguably the most critical, step in optimizing medical office workflow is to actually sit down and map the patient journey.
The patient journey is essentially the series of events and scenarios that the patient would typically go through before, during, and after their visit.
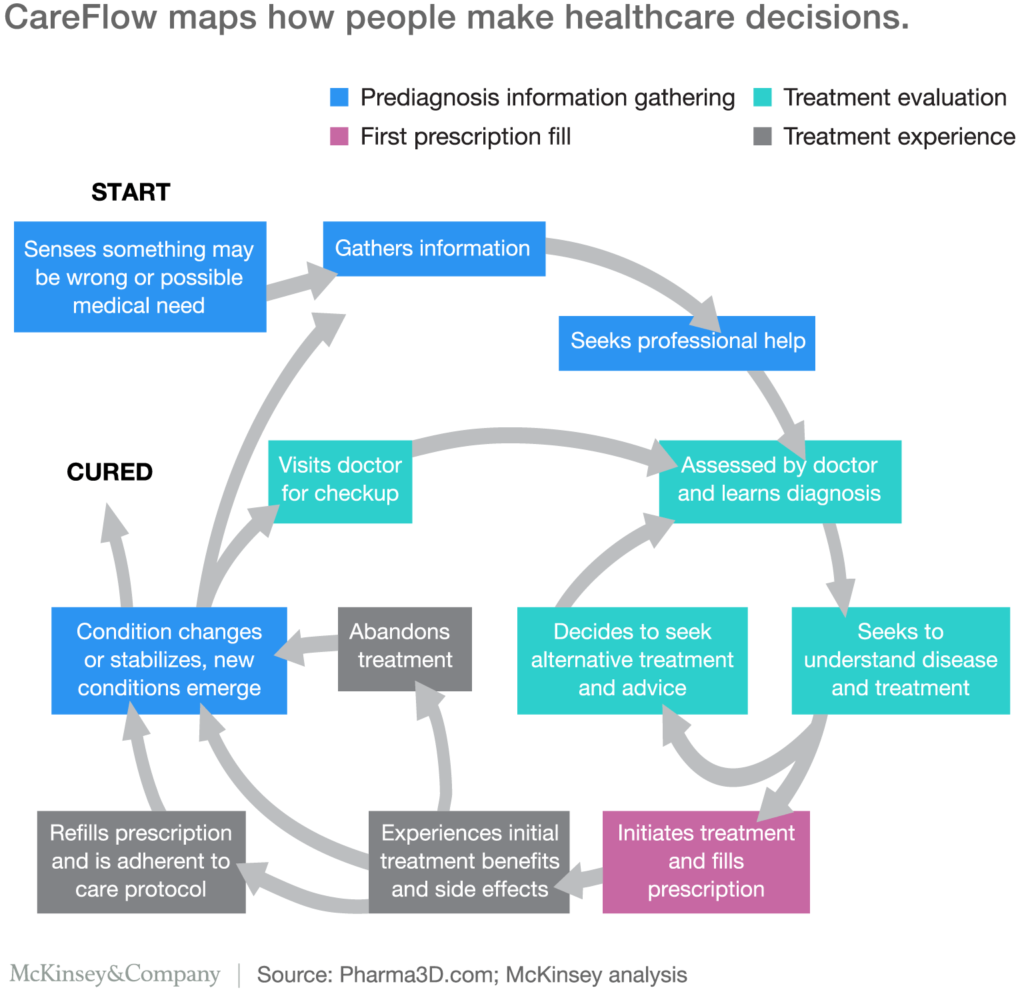
Most recently called a Care Flow Model, the patient journey is often a bit convoluted, but each step directly impacts the patient’s decision-making process and after-treatment actions.
For example;
- If you’re an urgent care clinic, your typical patient may begin their journey with a sudden and unexplained health issue, like a broken nose or persistent pneumonia.
- Their next steps would typically be to do a little internet research before visiting your facility.
- Once they’re in your facility, they will go through a series of intake procedures like filling out patient forms and insurance documentation.
- This information is then entered into your health record system.
- While they wait to be called, the patient will likely be reading available literature in the waiting room. Making this literature relevant to the patient’s needs is a good option.
- The patient is called into the exam room and is seen by an attending nurse or doctor on staff. Key points from their intake documentation are reviewed and a diagnosis is made.
- The patient exits the exam room and discusses next steps with the office admin while paying their co-pay or finalizing paperwork.
- The admin calls in the patient’s prescription if needed.
- The patient goes to pick up their prescription and heads home.
Now, this is a basic outline of what a lean patient journey might look like. However, there are often several steps that might be overlooked or skipped entirely by many organizations. But, this is not due to negligence, this is purely because they are not fully aware of how those additional steps impact the patient experience.

In this example, steps 3 through 8 are completely in your hands and should be broken down and optimized to ensure that they run smoothly, like a well-oiled machine. This not only maximizes the patient experience, but also results in a reduced risk of compliance failure.
Step 2: Assess the Current Situation and Pinpoint Any Overlap
Once you have a solid grip on how the patient moves through your facility, you’ll need to figure out what touchpoints are lacking or if there is any overlap in care.
Tasks – Outline what tasks are currently being performed during each stage of the patient journey. Are any of these tasks redundant or lack a purpose. There is no need to ask the patient the same question several times.
Team – Map the current responsibilities by team member and chart which tasks happen to fall within the responsibility of more than one team member. There’s no sense in doing the same thing more than once. Find out which team members are redundant and adjust their responsibilities to be more inclusive of the patient journey.
Tools – Inventory and outline your current technology and tools. Are there any tools that are redundant, out-of-date, or are rarely used? In the other vein, are there tools that are frequently used but may be missing a key element to be more useful?
Process – Do you actually have a process in place for key events like intake, treatment, prescription, and discharge? You should. Review your current processes and find out if there is any overlap or if any fall short.
Going through this process should give you a good idea of where your medical workflow is lacking and where to best optimize for best results.

Here’s a tip, try to leverage medical value stream mapping when performing this step to ensure that you are dotting every ‘i’ and crossing every ‘t’.
Step 3: Outline the Tools and Resources Need to be Effective
Now that you’ve spent the time to outline both the patient journey and shed some light on any gaps in your current process, it’s time to go over the tools of the trade.
There are many, many tools that are being used or can be used in a medical facility to optimize operational and treatment processes. But, are you using too many? Or, maybe you’re using too few?

During the last step, you took a look at your tasks, team, and tools. Hopefully, you realized that there are tools that are not quite pulling their weight. If that’s the case, here are a couple of options to streamline your tools and resources to be more effective:
Utilize Automation – Believe it or not, automation is a HUGE benefit to the healthcare industry. From automatic prescription dispensing services to automatic patient reminders, they simplify things throughout the entire patient journey.
In fact, here’s a rundown of how medical automation can actually improve doctor-patient relationships across the board.
Automation for your organization can come in many different forms, and you have to choose which one makes the most sense based on your findings in steps 1 and 2.
Adopt an Effective Centralized Record System – This may seem like common knowledge, but leveraging an effective centralized record system for your entire facility is a must.
If you discovered, in step two, that your current technology wasn’t quite hitting the mark, you may want to consider casting a wider net for a new solution that fully covers your bases.
Look for an EHR that accommodates all, or almost all, of your primary needs. Many of these systems are very comprehensive these days and can be made even more comprehensive with the addition of tools like Zapier and ITTT.
Integrated Point of Care Pharmacy Solutions
It may seem a little counterintuitive to integrate prescriptions into the actual treatment process, but it is actually incredibly beneficial to the overall patient experience, patient adherence, and a simplified workflow.
TIP: Here are 6 key benefits of an integrated point of care pharmacy solution for your facility.
Making prescription medication available prior to discharge allows your team to go through the motions of asking/answering questions, explaining medication usage and expectations, and ensuring that all the boxes are checked off on your treatment workflow checklist.

There are several options for integrating a point of care pharmacy solution, but not all are created equal. Take the time to do your research and make sure that your chosen solution makes sense for both your facility goals AND your customer needs.
While your tools and technology are pivotal to creating a streamlined treatment environment, the people are really what make the difference…
Step 4: Assign Roles Within Your Facility
Now that you know precisely what needs to be covered and which tools and resources you’re going to use to get there, it’s time to assign roles within your facility.
Using your patient journey map and process outline from steps 1 and 2, determine which staff members MUST attend certain steps. For example; the attending physician MUST have the final say on diagnosis and prescription. Then determine which steps can be consolidated under one umbrella of responsibility and as such be assigned to a specific person.

This step ensures that each and every task within your medical office workflow process is not only covered but efficiently covered with no overlap and no gaps.
It also ensures that everyone knows what their specific responsibilities are, which is key to enforcing the goals and expectations for those responsibilities.
Step 5: Set Expectations and Goals
While this step may seem simple, it is critical to maintaining consistency and compliance within your facility.
Once roles and responsibilities are established, lay down some ground rules for each of those roles. This sets the standard for treatment zone workflow processes and helps each team member keep their roles straight.
Two things to consider when establishing these goals and expectations:
- Document the specific expectations and actual responsibilities within each role.
- Make the goal achievement process fun with some simple gamification.
(i.e. Provide a reward for a specific number of patient discharge documents approved without error or adjustments. Or, institute an overarching reward for a patient readmission reduction of 1% per quarter.)

Step 6: Execute and Review
Once your new medical office workflow is documented and distributed, go ahead and roll it out. Be sure to schedule regular performance reviews to ensure that the new workflow is being followed and is performing as expected.
If not, repeat steps 1 and 2 to make sure that your patients and assets are where they need to be.
A Streamlined Medical Office Workflow is Only 6 Steps Away
While having an optimized treatment zone workflow is critical to compliance and patient experience, it doesn’t have to be hard to achieve it. Simply follow steps 1 through 6 above to improve your internal processes and better serve your patients from intake to discharge.
Do you happen to have an insider tip on improving your medical office workflow? We’d love to hear about it! Share your insights with us in the comments below.
If you’re interested in learning more about how integrated point of care pharmacy solutions, like the medifriendRx® prescription kiosk, can improve workflow AND increase revenue, request a demo today.